Which is the role of the unknown in contemporary Medicine? Can Philosophy provide some help in dealing with it? [Foundazione ISTUD] publishes an interview with Dien Ho, PhD, Associate Professor of Philosophy and Healthcare Ethics, Director of the Centre for Health Humanities at Massachusetts College of Pharmacy and Health Sciences (MCPHS) in Boston….
[Dien Ho]: In order to identify the aetiology of disease and potential treatments for them, we have first to determine that the physiological presentations are in fact pathological. In other words, whether some human condition constitutes a disease or not is a question we must answer prior to exploring how [Evidence-Based Medicine] can help us tackle them. The definition of disease (and relatedly health) is not a simple biological matter. There are plenty of “normal” biological functions that we pathologize and treat….
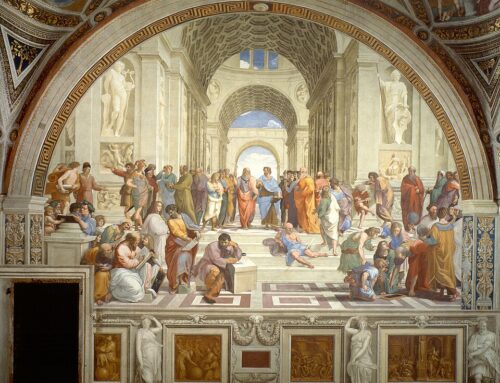
The categorization of a condition as pathology must be determined extra-biologically. No amount of empirical research in clinical trials can possibly answer the question for us. In this sense, before EBM becomes relevant, we must ask some basic social and philosophical questions regarding the pathologization of a condition. This is particularly germane since the medicalization of human conditions has been a growing phenomenon since the advent of modern medicine. Our increasing ability to control physiology can easily tempt us to the conclusion that human conditions must be controlled. It behoves us to keep in mind that pathologization has historically been often guided by social norms, bigotry, and financial incentives….
Placebos are fascinating for me because they seem to challenge the way we practice clinical medicine. Ultimately, there is really nothing mysterious about placebos. Whenever someone says placebos are about mind over body, I point out that your mind is also your body (Cartesian dualism notwithstanding): placebos are really about body over the body. To be sure, placebo effects are likely all in your head but then, again, so is your brain.
The existence of placebo effects strikes me as rather well established, especially in terms of their analgesic power. A common criticism of placebos is that they are only effective for “subjective” conditions such as pain, anxiety, and fatigue (outcomes that depend largely on patients’ reports) but that they are ineffective for “objective” conditions. A few things to keep in mind. Firstly, there are some studies that show placebos can have remarkable effects on “objective” conditions such as T-cell count, mobility, and blood pressure. One of the most incredible cases I read involves a young man who, in an attempt to commit suicide, ingested all the anti-depressants that were given to him in a clinical trial. His blood pressure dropped to 80/40, and he needed fluid infusion in order to maintain normal pressure. The attending in the emergency room contacted the principal investigator of the study and learned that the young man was in fact, in the placebo arm of the study. Instead of ingesting anti-depressants, he had ingested 29 placebo pills. Within 15 minutes of learning of the news, his blood pressure rose back to 120/80. The case review describes the young man as having overdosed on placebos. Similar “objective” results have been noted in cases of sham surgeries in which clearly indicated fractures had not been treated, but patients regained mobility.
Secondly, the dismissal of placebo as being entirely subjective stems from modern medicine’s myopic focus on “measurables”. Not only do we ask patients how they feel as a way to assess the effectiveness of a treatment, but it also shifts clinical attention away from alleviating patients’ discomfort to obsessing over numbers. The bias to treat and the bias to medicalize, I suspect, come partly from our emphasis on numbers….
One thing that I learned from my research on placebo is how much of the therapeutic benefits of modern medicine depends on certain performative. From how we label a drug to the colour of a pill, from the belief in the therapeutic benefits of medicine to a clinician’s outfit, subtle features of the healing environment contribute to therapeutic effectiveness. Indeed, rather than thinking there is a distinction between the healing environment (a doctor’s office, her demeanour, one’s trust in medicine, etc.) and the intervention itself (chemotherapy, antibiotics, physical therapy, etc.), it is better to think of the entire healing experience as one large unit with no significant distinction between the context and intervention. Placebos have typically been relegated to the contextual part of the therapy. If the picture I am proposing is correct than the line between placebos and standard treatments does not exist. At the end of the day, what matters is improving patients’ well-being; how much of it is due to the context and how much of it is due to the intervention is not only unimportant, it is in principle impossible to discover (as I have argued elsewhere).
For other articles on narrative medicine, see here.



Leave A Comment